- The TriDoc Podcast-in Supplement form
- Posts
- Episode 180: Lumos sleep mask/Pavlos Antoniades
Episode 180: Lumos sleep mask/Pavlos Antoniades
A brief synopsis of the episode's main discussions and takeaways as well as extended references
In this episode, we examined some tech to help you sleep and shift your circadian rhythm when traveling and I spoke with an up and comer on the Canadian National Development team for triathlon who also happens to be a medical student. What is it with multisport and overachievers??!!
Table of Contents
Lumos sleep mask-a worthy bit of tech to help you sleep or just an overpriced eye shade?
In evaluating the Lumos, a $299 (on sale for $249 at the time of writing) sleep mask that includes an LED panel, we first reviewed the why and how around light therapy for adjusting circadian rhythm. There is a growing body of research that supports the theory that light has a big role in keeping our brains in sync with the day wherever we may be. This explains why shifting to a new time zone can be difficult. We need time for our minds to recalibrate to the new light/dark cycle. By leveraging very bright light for short periods of time, scientists have found that you can hasten that adjustment. The Lumos light mask makes use of this knowledge and converts it to a wearable solution. But does it work? Their website gives some pretty good results but independent research was hard to come by. In the end, the science and the user reviews are compelling and I decided that I would bite the bullet and take one for the team and get one to experiment as an N of 1 and report back in a future episode!
Pavlos Antoniades, the latest overachieving medical student who also is a nationally recognized triathlete
About Pavlos from his World Triathlon bio : Like many Canadian kids, Pavlos played hockey until he was 11 years old but had a passion for many other sports including soccer, tennis and golf. In the winter, he still can be found alpine and cross-country skiing. But his focus since he was eight years old has been on triathlons, following in the footsteps of his dad and siblings. He began using triathlon as a strong cross training for hockey, but quickly chased a new sport career path where he has been making steady progress in both domestic and international racing. He has represented Canada at the 2017-2018 and 2019 Junior World Championships. When not training or competing, Pavlos studies medecine at University of Montreal and enjoys playing music.

The episode takes a turn into the unpredictable world of triathlon racing and medical education, featuring the inspiring yet chaotic life of Pavlos Antoniades, who manages to balance the demands of being a medical student with the intense training required for elite triathlon competitions. It’s not just a chat about sports; it’s a reflection on the extreme realities of time management and the mental toughness needed to survive both worlds. Pavlos vividly shares his journey from playing hockey to dominating in triathlon, illustrating the relentless quest for excellence that drives him. We explore the challenges he faces in maintaining a rigorous training schedule while also hitting the books hard—exams, internships, and all the stress that comes with them. As he nears the end of school, he faces a tough choice. Will he take a year off to chase Olympic dreams, or will he dive headfirst into residency? Join us as we navigate the highs and lows of this extraordinary journey.
Episode takeaways:
Finding a viable routine is key for balancing triathlon training and life commitments.
The integration of training and school requires meticulous planning, especially during exams.
Light therapy products like the Lumos sleep mask show promise, but user experiences vary significantly.
Managing fatigue during travel and training is a constant balancing act for aspiring athletes.
References used for the MMB
Question: Is the Lumos Mask effective?
Overall
Most light therapy studies focus on older adults
While light has the capacity to advance/delay circadian rhythms of melatonin, core body temperature, and corticosteroids, showing promise for the use of light for the treatment of sleep disorders, discrepancies exist in research results
The first meta-analysis examining the effect of light therapy on overall sleep disorders and specific conditions shows small to moderate positive effects.
However, publication bias has been observed
Studies suggest blue light is more effective than longer wavelengths, like green light, to reset the circadian rhythm, suppress the nighttime release of melatonin, and enhance performance.
This article reports that the efficacy of light therapy depends on the dose of light stimulus.
Laboratory and field studies indicate that light should be 2,000-10,000 lux to elicit a clinically significant response and also short enough (<2 hours) to ensure patient compliance.
Some articles report suggested dosage, but others suggest dosage should be deferred to clinical judgement
Lumos Tech sleep mask ($249 - $299) is primarily designed to shift the circadian clock for night shift workers and jet lag, rather than for clinical conditions
It is reportedly scientifically designed
Mixed reviews about the fit of the mask found online, including issues of gaps between the mask and the under-eye area
According to studies of flash light therapy, the potential for the light mask application to solve jet lag for work shift problems are shown by the effect of light therapy on delaying the secretion of melatonin by 0-6 hours following 1h exposure.
However, studies report high variability in flash light therapy response.
Lumos Smart Sleep Mask
Product website
Key Points:
The purpose of this mask is to improve well-being by improving sleep
The Lumos sleep mask is reportedly scientifically designed to use light therapy to regulate one’s circadian rhythm by resetting the internal clock
The goal is to regulate hormones, including melatonin
Used to:
Beat jet lag
Transition for night shifts
Optimize sleep
Wake up early
Reset for Monday
Daylight saving time
Users select a program, input their schedules, and wear the mask as instructed by the program
The website claims that decades of research from Stanford University demonstrate that brief light flashes are effective for regulating circadian rhythms
This product development is reportedly supported by NASA, DoD, and NSF
The product appears to have been tested in multiple lab and real-world studies
The website references 9 publications by Dr. Heller and Dr. Zeitzer, who is an uncompensated scientific advisor to LumosTech
Website notes:
Clinical study participants reported on average 70% reduction of night shift fatigue.
Study participants demonstrated up to 37% reduction in time to fall asleep.
On average 46% reduction in jet lag was reported by testers in the travel field study.
The sleep mask is only compatible with iOS devices
Opening on the side of the mask for LED module removal
USB-C charging
On the website, the mask is sold for $299 and discounted to $249
Bright Light Therapy
Stanford Medicine Website
Key Points:
Bright Light Therapy, also known as phototherapy, is used to shift sleeping patterns
Properly timed light exposure is given to adjust a patient’s biological clock
Both artificial and natural light can be used
Therapy is used to manage circadian rhythm disorders, with sleep specialists typically working with individual patients to plan the light exposure in accordance with their symptoms and life circumstances
Used to treat various sleep syndromes, such as those where individuals face difficulties waking up in the morning due to not falling asleep until hours past midnight
The degree of success of the therapy varies per patient
There is variability in the data available to assess the effectiveness of light therapy for different conditions
Illuminating Rationale and Uses for Light Therapy
Shirani and St. Louis (2009)
Key Points:
This publication in the Journal of Clinical Sleep Medicine is not an industry-supported study
This paper explains circadian rhythm as a self-sustaining biological activity oscillating with a periodicity near 24 hours, which tends to move in synchrony with environmental rhythms
The mammalian “master biological clock” is located in the paired suprachiasmatic nuclei of the anterior hypothalamus
Genetic mutations and lesions in this region have been associated with disrupted circadian rhythms of hormones and complex behaviors
“Entrainment” is the setting of the biological clock
While the intrinsic human circadian period is 24.2 hours, environmental zeitgebers (mainly light-dark stimuli) prevent drifting and divergence from the 24-hour terrestrial day
Light-sensitive receptors in the retina mediate the light-dark cycle and its effect on the central nervous system

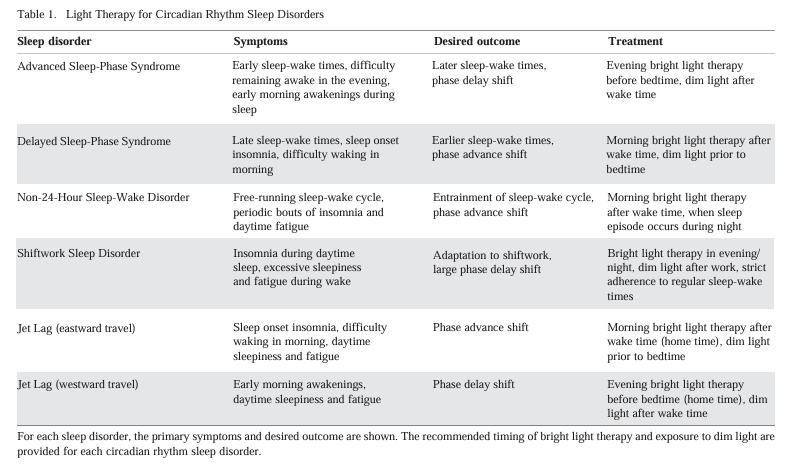
(Fig. 1 from paper)
Light therapy aims to reset this biological clock using the light-dark cycle:
Synchronize the sleep-wake cycle with the subjective night
Shift the biological clock phase to facilitate sleep at a desired time of day/night
Advance the biological clock phase to attain indirect effects on mood
Light administration correlates with changes in the plasma/salivary concentration of melatonin
Light has the capacity to advance/delay circadian rhythms of melatonin, core body temperature, and corticosteroids
Some light therapy used for therapeutic interventions has not been tested
Optimal duration of light therapy not yet established
This article reports that decisions about dosage must be deferred to clinical judgement
2500-12000 lux light is 1-3 feet from patient
Light should be positioned above eye level since the lower area of the retina has a greater tendency to communicate the biological clock

The effects of light therapy on sleep problems: A systematic review and meta-analysis
Maanen et al. (2016)
Key Points:
The effect of light on the suprachiasmatic nucleus (SCN), a region of the brain that controls circadian rhythms, its role in inhibiting the secretion of melatonin, and its effect on the ascending arousal system make it promising for use in treating sleep disorders.
This meta-analysis was the first publication that systematically reviewed the effects of light therapy on sleep problems in general and on specific types of sleep problems.
They report that the research on the effect of bright light therapy shows small to moderate effects, smaller than the effect of cognitive behavioral treatments on insomnia reported in past studies
Multivariate analysis of 53 papers with 1154 participants showed significant effects of light therapy for sleep disorders in general (g=0.39), for circadian rhythm sleep disorders (g=0.41), insomnia (g=0.47), and sleep problems related to Alzheimer’s/dementia (g=0.3).
Only early morning awakening did not show significant results
Largest effect sizes found for circadian outcomes and insomnia symptoms.
Smaller effect sizes found for RCT studies
Publication bias found for 5/13 sleep outcomes with published studies differing from unpublished studies
Unexplained variability in data existed even after the moderators were assessed.
Methods: 2-phase literature search was conducted in November 2012 and March 2015 with RCT filter. Sleep conference proceedings were also searched. Experts contacted for unpublished papers. Included in analysis if participants were included based on sleep disorders or complaints, light intervention was used to treat complaint, at least 5 participants involved, and in English. Study with participants in senior homes excluded. Hedges’ g effect calculated. Egger’s test conducted for publication bias.
Results: First literature search yielded 3159 unique results. Second search yielded 805 new results. 53 studies included. 1154 participants involved. Significant effects of light therapy observed for combined sleep disorders and for CRSD, insomnia, problems related to Alzheimer’s/dementia, and other sleep problems. Significant effect was not found for early morning awakening. Light therapy was found effective in the treatment of sleep problems in general (g=0.39), and for circadian rhythm sleep disorders (g=0.41), insomnia (g=0.47), and sleep problems related to Alzheimer's disease/dementia (g=0.30). Smaller effects for circadian rhythm sleep disorders were observed for randomised controlled trials. Egger’s test for publication bias indicated that 5/13 outcomes had indication of publication bias, showing circadian (t (20)=3.34,p<0.01), bedtime (or sleep onset time) (t(22)=3.04, p<0.01), wake after sleep onset (t(23)=2.18, p=0.04), sleepiness (t(22)=2 .36,p=0.03), and sleep quality (t(17)=2.79,p=0.01). No studies on children found.
Treatment of Circadian Rhythm Sleep Disorders with Light
Gooley (2008)
Key Points:
In circadian-rhythm disorders, misalignment in sleep-wake patterns causes insomnia, fatigue, and deteriorated performance.
This article reviewed laboratory and field studies that established bright light therapy treatment to be effective and examined the physiological basis for bright light therapy to provide guidelines for the appropriate use of light therapy.
Studies suggest that exposure to blue light is more effective than longer wavelengths, like green light, to reset the circadian rhythm, suppress the nighttime release of melatonin, and enhance performance.
This article reports that the efficacy of light therapy depends on the dose of light stimulus.
Laboratory and field studies indicate that light should be 2,000-10,000 lux to elicit a clinically significant response and also short enough (<2 hours) to ensure patient compliance.
Eye exams should be done prior to light therapy use to ensure normal ocular health and caution should be taken if photosensitizing medications are taken.
Moving time zones in a flash with light therapy during sleep
Lok et al. (2023)
Key Points:
This study assessed the efficiency of flash therapy during sleep to shift the circadian clock
Flash therapy, noted for its potential to be at least twice as effective in phase-delaying the circadian clock, exposes one to a sequence of light flashes instead of continuous exposure
In the presence of flashes, the circadian system is reported to be more sensitive to lower light intensities
During sleep, light must pass through eyelids, reducing light by 86-97%
This study did not include participants with sleep disorders.
Study demonstrated that 1h flash exposure (~1200 lux 2-ms flashes of broad-spectrum white light every 15s. ), timed at the beginning of sleep, can significantly phase delay the circadian clock 1.13 ± 1.27 h on average (ranging from 0 to 6.15 h) compared to minimal change of (12±20 min) for the control with goggles but no flashes.
While significance remained after phase-controlled analysis, large variability in results were observed between participants.
Light therapy did not alter the micro- or macro- sleep architecture as seen by consistencies in duration of each sleep stage and frequency of transitions between phases.
Significant difference observed for amount of delta power during flash/placebo may be due to capturing of event-related potential, but no significance was observed depending on sleep stages.
This paper notes that “while it is possible that the PRC to flashed light is different from the PRC to continuous light, this is more likely to be in the magnitude rather than the shape of the curve.”
The highly variable response to flashed light is consistent with reports in other species and may be due to the probabilistic nature of photoreception, converting electromagnetic to electrochemical signal, where some flashes may not activate retinal circuits.
Lumos mask not mentioned in study
Methods: Healthy young participants (N=10, females n=5, males n=5) with normal color vision involved in randomized, placebo-controlled experiment. No evidence of sleep disorders, depression, medication with potential to impair sleep, or alcohol disorder. Within-subject study. 2 week at-home sleep monitoring before laboratory stay, where wake time, bedtime, and sleep latency was self-reported. Participants instructed 7-9h sleep/night. Wrist-worn actigraphs monitored compliance and objective sleep timing. Rescheduled if >30min deviation from target observed 2+ days. Caffeine intake refrained 1 day before lab. 37h laboratory portion with controlled lighting in room. Saliva sample collected periodically. 1h light stimulus starting 30min after HSOn. ~1200 lux 2-ms flashes of broad-spectrum white light every 15s. Salivary melatonin onset assessed.
Results: Demonstrated that 1h flash exposure for 1h, timed at the beginning of sleep, can phase delay the circadian clock 1.13 ± 1.27 h on average (ranging from 0 to 6.15 h) compared to minimal change of (12±20 min) for the control group who had goggles but no flashes. Significant difference between therapy and control (F(1,2)=6.44, P<0.01) with a large effect size (d=1.02). Variability in results by participant with 2 showing no change, 3 showing modest change (<1h), 2 showing moderate change (1-2h) and 2 showing large change (>2h) potentially due to variability in phase angles of stimulation. Phase-corrected data also showed a significant large effect (d = 0.93). No significant difference in duration spent in W, N1,N2, N3, or REM, as well as number of N2/N3 transitions or transition to REM. Significant difference observed for amount of delta power during flash/placebo, but not observed depending on sleep stage.Not a subscriber to the podcast? Click here!
Support the podcast: TriDoc Podcast Patreon site
Need an endurance coach? TriDoc Coaching
Reply